Ovarian Cancer
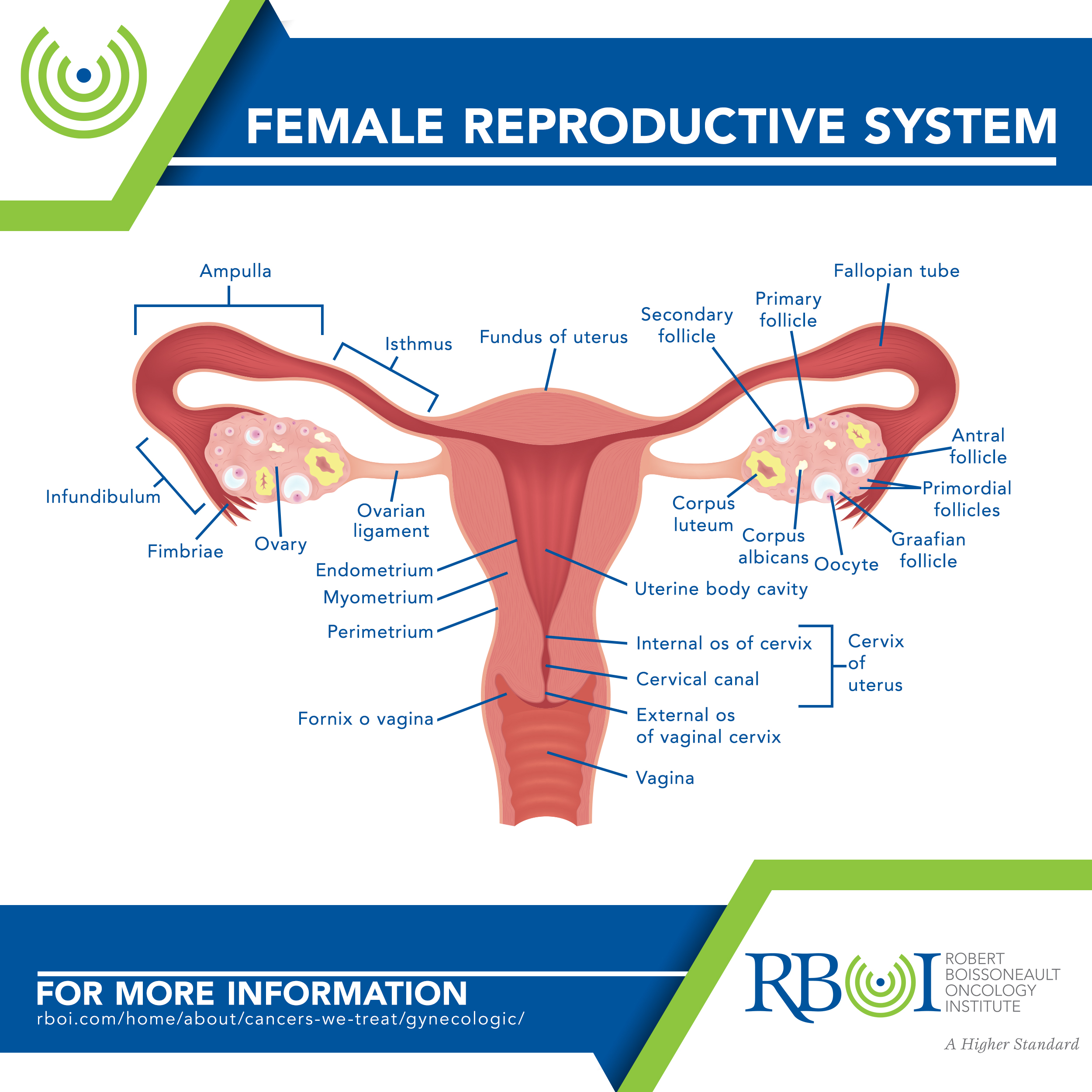
Ovarian cancer includes cancers that begin in the cells in the ovary, fallopian tube, or (rarely) peritoneum. The cancers are closely related and are treated the same way. They also tend to be aggressive.
-
Forms of ovarian cancer
Epithelial ovarian tumors account for 85 to 90 percent of ovarian/fallopian tube cancers. These tumors start from the cells that cover the outer surface of the ovary.
Germ cell tumors start from the cells that produce the eggs (ova) and are uncommon. They tend to occur in females aged 10 to 29 years.
Stromal tumors are rare. They start from structural tissue cells that hold the ovary together and produce the female hormones estrogen and progesterone. More than 90 percent of these tumors start in granulosa cells.
-
Risk factors for ovarian cancer
Age, Endometriosis, Ethnicity, Family history of ovarian cancer, Hereditary cancer syndrome, History of breast cancer, Hormone replacement therapy, Reproductive history, Weight
Age — Most ovarian cancers develop after menopause. Half of all ovarian cancers are found in women 63 years of age or older. This cancer is rare in women younger than 40.
Endometriosis — Researchers are studying whether endometriosis is a risk factor for ovarian cancer. It may increase the risk of certain types of ovarian cancer, including clear cell and endometrioid ovarian cancers.
Ethnicity — Women of North American, Northern European, or Ashkenazi Jewish heritage have an increased risk of ovarian cancer.
Family history of ovarian cancer — Your ovarian cancer risk is increased if your mother, sister, or daughter has (or has had) ovarian cancer. The risk also gets higher the more relatives you have with ovarian cancer. Increased risk for ovarian cancer can also come from your father’s side. Increased risk has also been linked to a family history of colorectal and breast cancer.
Hereditary cancer syndrome — About 5 to 10 percent of ovarian cancers are a part of family cancer syndromes resulting from inherited changes (mutations) in certain genes. These syndromes include hereditary breast and ovarian cancer syndrome, PTEN tumor hamartoma syndrome (also called Cowden disease), hereditary nonpolyposis colon cancer (also called Lynch syndrome), nevoid basal cell carcinoma syndrome (also called Gorlin syndrome), Peutz-Jeghers syndrome, Li-Fraumeni syndrome or ataxia-telangiectasia, and MUTYH-associated polyposis. Research is ongoing to see if other hereditary syndromes may be linked to ovarian cancer.
History of breast cancer — If you have had breast cancer, you might also have an increased risk of developing ovarian cancer. The risk of ovarian cancer after breast cancer is highest in those women with a family history of breast cancer.
Hormone replacement therapy — Women who have taken estrogen-only hormone replacement therapy (HRT) after menopause, for at least 5 or 10 years, may have a higher risk of ovarian/fallopian tube cancer. The risk increases the longer a woman uses the therapy and decreases over time after the therapy ends. This increased risk is less certain for women taking both estrogen and progesterone.
Reproductive history — Women who have their first full-term pregnancy after age 35, who never had a child, or who have not taken birth control pills have a higher risk of ovarian cancer.
Weight — Recent studies show that women who were obese in early adulthood have an increased risk to develop ovarian/fallopian tube cancer. Obese women (those with a body mass index (BMI) of at least 30) may have a higher risk of developing ovarian cancer, but not necessarily the most aggressive types, such as high grade serous cancers. Obesity may also affect the overall survival of a woman with ovarian cancer.
-
Factors with unclear effects on ovarian cancer risk
Androgens — There appears to be a link between certain androgens (male hormones) and specific types of ovarian cancer, but further studies are needed.
Fertility treatments — In vitro fertilization (IVF) seems to increase the risk of the type of ovarian tumors known as “borderline” or “low malignant potential.” Although fertility drugs were once thought to increase the risk of ovarian/fallopian tube cancer, no increased risk has been found.
Talcum powder — Findings have been mixed as to whether talcum powder applied to the genital area is linked to ovarian cancer.
-
Symptoms of ovarian cancer
The most common symptoms of ovarian cancer can include:
Bloating
Pelvic or abdominal (belly) pain
Trouble eating or feeling full quickly
Urinary symptoms, such as urgency (always feeling like you have to go) or frequency (having to go often)
These symptoms tend to be persistent, occurring more often and being more severe. Other symptoms of ovarian cancer can include:
- Pronounced fatigue
- Upset stomach
- Back pain
- Pain during sexual intercourse
- Constipation
- Menstrual changes, such as heavier bleeding than normal or irregular bleeding
- Abdominal (belly) swelling with weight loss
- Vaginal discharge, which may be clear, white, or tinged with blood
-
How is ovarian cancer treated?
Radiation therapy is not used as a first treatment for ovarian/fallopian tube cancer. Occasionally, it can be an option for treating small, localized recurrent cancer.
Intraperitoneal radiation therapy is being studied in clinical trials to treat advanced ovarian cancer. In this treatment, radioactive liquid is placed directly in the abdomen through a catheter.
Click here to learn more about RBOI’s radiation treatment options
Click here to watch a walk-through of what is involved in radiation treatment at RBOI
More extensive information about ovarian and other cancers may be found at these sites:
American Cancer Society: Cancer.org
American Society of Clinical Oncology: Cancer.net
National Cancer Institute: Cancer.gov
